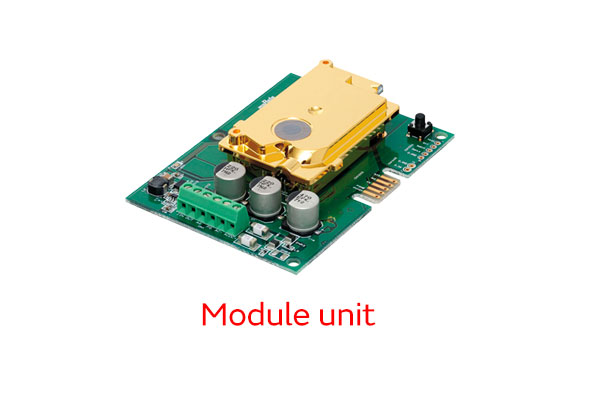
CO2 sensor
The COVID pandemic that began in 2020 is showing no signs of coming to a close. For society to recover and progress in this post-pandemic era, the thing we need most is to reduce the risk of infection at schools, offices, and other places where people gather. The key is avoiding the three Cs: closed spaces, crowded places, and close-contact settings. It is especially important to avoid closed spaces, something we can accomplish through proper ventilation, to prevent aerosol transmission (airborne infection). In the first part of this two-part series, two Murata Manufacturing employees—Mr. Imagawa, who is in charge of spatial visualization solution development, and Mr. Dan, who is in charge of CO2 sensor development—asked Dr. Yo Ishigaki, a project associate professor at the graduate school of the University of Electro-Communications, about the need to measure CO2 concentration to serve as an indicator for ventilation, methods of visualizing air quality, and more.
--The National Institute of Infectious Diseases has published its views on how COVID-19 is transmitted. What is your opinion?
Dr. Ishigaki: My opinion is centered on the idea that the list of infection routes starts with aerosol transmission, when people inhale virus-laden particles from the air. People have been saying this for quite some time in other countries. Even so, it carries great weight when a country’s official institute of infectious diseases recognizes aerosol transmission. The National Institute of Infectious Diseases provided several pieces of evidence in its recognition of aerosol transmission. For example, the virus spreads widely within airplanes and to every corner of restaurants, even between strangers. In other words, the virus is passing between people who are seated far apart and have no direct contact with each other. Aerosol transmission is the only way to explain this phenomenon.
Imagawa: Once aerosol transmission is identified as a cause of infection, control measures change as a matter of course, don’t they?
Dr. Ishigaki: Yes, the national government may decide to change the policy. For example, the basic strategy to date cannot remain unchanged when dealing with subsequent waves of infections. What we need now is to wear masks and make every effort to ensure proper ventilation. Changes to basic strategies obviously have downstream effects, for example how subsidies are given. In retrospect, we believe that aerosol transmission was already occurring when the Delta variant appeared, but that the viral load of exhaled breath rose sharply with the Omicron variant.

--If aerosol transmission is the primary factor in outbreaks, doesn’t that change what we should focus on when avoiding the three Cs?
Dr. Ishigaki: Of the three Cs—closed spaces, crowded places, and close-contact settings—closed spaces are the most problematic for aerosol transmission. We have studied the relationship between closed spaces and transmission at elderly care facilities, schools, and production floors, to cite some examples. Aerosol transmission was believed to be widespread at each of the places we studied. For example, infections were spreading at elderly care facilities despite the administration of vaccines and best efforts to ventilate from the early stages. The reason for this is airflow.
Dan: Airflow may indeed be a blind spot.
Dr. Ishigaki: In one elderly care facility where a cluster occurred, the first positive patient lived alone in a single room. However, just outside the patient’s room was a day room where other residents gathered. The day room was equipped with a powerful ventilation fan, so ventilation was not considered to be a problem. Unfortunately, the ventilation in the day room was too powerful and pulled air from the positive patient’s room. In other words, even though the facility was well ventilated, infections spread because airflow was not rigorously controlled. Given what happened in this example, from now on we need to be mindful of airflow when taking steps to ventilate spaces.
--What about factories and other places where airflow may be problematic?
Dr. Ishigaki: At one factory, a fan happened to be blowing air right at a positive patient, and the virus spread through the patient’s work area. An ideal environment would feature a structure like the clean rooms you probably have at Murata Manufacturing—that is, a space where super-clean air is forced in through the floor and constantly circulated.
Imagawa: Your published research includes a case of a cluster originating from a plastic sheet.
Dr. Ishigaki: Yes, in this case, a plastic sheet was used to screen off an area from up near the ceiling to the floor, blocking ventilation and resulting in infections. Plastic sheets are effective shields for preventing droplet transmission, but should not be used to screen off areas if aerosol transmission is to be considered. Apparently, our report has led some local governments to change their guidelines and responses. In considering airflow, we need to think about another aspect of ventilation: energy conservation. There is a tradeoff between ventilation and energy consumption. In that sense, it is necessary to monitor ventilation.

--If a building is properly designed in line with the Building Standards Act of Japan, is it safe to assume that there are few problems with ventilation in its current state?
Dr. Ishigaki: It is not safe at all because many buildings are not properly ventilated. A survey of around 100 places of business in Tokyo revealed poor ventilation in around half. CO2 concentration measurements regularly showed 3,000 ppm—and even topped 10,000 ppm in some cases—compared with the standard of 1,000 ppm or lower. The concentrations were so high because the buildings lacked ventilation to begin with, or filters were clogged, or existing ventilation was malfunctioning. Under specific laws, buildings like these should fall under the category known as “existing nonconforming”, but have not explicitly been placed in that category for various reasons. One such reason may be that building ventilation is overseen by the building guidance section of a prefectural or municipal government rather than the public health center. This is a textbook example of a government silo and its pitfalls, but something must be done to break it down because viruses thrive where defenses are weak. What we need are systems that constantly measure CO2 concentration.
--What makes CO2 concentration a good indicator of ventilation?
Dr. Ishigaki: It’s a good indicator because CO2 is contained in the air we exhale, as are viruses. People constantly emit a lot of CO2. This is the natural result of the body burning oxygen within cells to gain energy. For example, if there are many people in a small room that is left unventilated, the CO2 concentration will increase rapidly. Thus, the CO2 concentration of a room is a good indicator of the total amount of air exhaled by its occupants. If people infected with the virus are among the occupants, the viral load of their exhaled breath should be proportional to the CO2 concentration of the room. This is why CO2 concentration is a proxy indicator of the risk of aerosol transmission. Epidemiological studies are forthcoming, but it is believed that better ventilation and lower indoor CO2 concentrations will reduce the risk of infection. In the case of tuberculosis, another disease transmitted aerially, studies show that keeping the indoor CO2 concentration at or below 1,000 ppm results in a 97% reduction of positive patients.
Dan: So if you stay in a car with the windows closed for a long time, the CO2 concentration will increase.
Dr. Ishigaki: I believe that CO2 is a contributing factor to accidents that occur immediately after taxi drivers take breaks inside their cars. When the engine of a car is turned off and the windows are closed, the CO2 concentration inside the car increases to around 8,000 ppm. This may put the driver into a bit of a haze, although they may not realize it. We conducted an experiment in which we asked professional drivers to solve simple problems while driving in a simulator vehicle with a CO2 concentration of 5,000 ppm and, as expected, found that they were significantly slower to answer and made mistakes at levels above 5,000 ppm. In fact, CO2 concentration also affects learning efficiency in schools; studies show that cognitive ability is significantly impaired if the concentration exceeds 1,000 ppm. That is the extent to which CO2 concentration affects cognition. So in places like schools, we should keep the air fresh at all times, not only to prevent infection, but also to maintain intellectual productivity.

--Timing seems like a concern when ventilating school classrooms.
Imagawa: The first step toward proper ventilation is to accurately measure CO2 concentration. Our spatial visualization solution AIRSual features an algorithm that predicts changes in CO2 concentration, making it possible to predict, for example, how long it will take for the concentration to reach 1,500 ppm. With that information, teachers should be able to ventilate classrooms when the time is right, even if it comes about during class. A demonstration experiment conducted at elementary and junior high schools in one municipality with the approval of its board of education revealed that the CO2 concentration in classrooms increases differently depending on the nature of the class.
--Do the differences occur depending on what the students are doing?
Dr. Ishigaki: Differences rooted in activity are also seen in restaurants. CO2 concentration increases during preparation time before opening and clean-up time after closing. This is because fans are turned off when there are no customers present, and also because employees enjoy talking with each other while cleaning up. CO2 concentration increases when people talk a lot without ventilation. This is why it is advisable to constantly monitor the CO2 concentration.
--That seems like it would require meticulous attention in elderly care facilities, though.
Dr. Ishigaki: The windows in elderly care facilities are typically designed not to open in order to prevent hazards such as patients falling out of them. This makes it impossible to ventilate naturally by opening windows. Moreover, in many cases, following design guidelines results in structures conducive to meandering in circles. This is done for several reasons, including to increase opportunities for residents to meet each other and to ensure that residents with dementia cannot wander off and end up somewhere far away. In these structures, people tend to gather in places like the corners of hallways. When this happens, people stay put and air stagnates, which is counterproductive as an infection control measure. Thus, proactive ventilation is necessary. Constant monitoring of the CO2 concentration is necessary to accomplish this.

Dr. Yo Ishigaki
Dr. Ishigaki is an expert in risk informatics. He studies methods of measurement and visualization to help people perceive risks correctly. He received a doctorate in engineering from the University of Electro-Communications and a master’s degree in art from Tama Art University. He researched and developed security systems for 10 years at SECOM Intelligent Systems Laboratory. Afterward, he commercialized Pocket Geiger, the world’s first smartphone-connected radiation detector; Pocket PM 2.5 Sensor, a device that visualizes air pollution; and Pocket CO2 Sensor, a device for visualizing the three Cs. He has also developed many pieces of medical and sanitary equipment. Dr. Ishigaki has received numerous awards, including the Minister of MEXT Award of the Local Commendation for Inventions, the Japan Prize, the Heisei Memorial Research Grant Award, the Good Design Award, and the RedDot Design Award. He has made numerous media appearances, calling for risk-averse behavior to prevent aerosol transmission.
Design for Humanity (Japanese only)